The Menopause Society’s Meno 101 education track brought together leading clinicians and researchers to provide a foundational — and refreshingly pragmatic — overview of menopause care. What stood out most is how rapidly guidance is evolving across hormonal, non-hormonal, behavioral, and digital care models.
For an era where patients increasingly show up with data in hand and a desire for shared decision-making, these sessions underscored a simple truth: menopause care must become as personalized and proactive as the women seeking it. That’s exactly the future Amissa is building toward — empowering clinicians with clearer symptom data, wearable insights, and actionable guidance in real time.
Below is a quick recap of the presentations, who led them, links to their slide decks, and one key takeaway from each.
Primary Ovarian Insufficiency & Early Menopause
Presenter: Dr. Cynthia Stuenkel — Clinical Professor of Medicine, Endocrinology and Metabolism, UC San Diego School of Medicine' Slides → Meno 101 Stuenkel slides.pdf
What was covered Dr. Stuenkel outlined the diagnostic evaluation for women under 40 with irregular cycles or secondary amenorrhea and emphasized early identification of POI to support fertility planning, symptom relief, and risk reduction for long-term health conditions.
Key takeaway POI is not just “early menopause” — it requires a targeted diagnostic workup (HC-G, FSH ± repeat testing, estradiol, TSH, prolactin) and proactive symptom and bone-health management. Early detection enables earlier support.
Where Amissa fits Tracking menstrual cycle changes, vasomotor symptoms, mood, and sleep — alongside wearable physiology — can help flag early risk patterns and alert clinicians sooner.
Genitourinary Syndrome of Menopause (GSM) 101
Presenter: Dr. Caroline Mitchell — Massachusetts General Hospital Slides → Meno 101 Mitchell slides.pdf
What was covered Prevalence of vaginal dryness, pain with sex, and urinary symptoms is high — yet underreported. Both hormonal and non-hormonal options are effective, but persistence is low without guidance.
Key takeaway Ask early. Focus on symptoms, not appearance. Half of women are already self-treating with OTC options that could make symptoms worse. Clinical screening and patient education are essential.
Where Amissa fits Symptom-tracking empowers clinicians to measure treatment response and engage patients in adjusting care plans — especially important for sexual health conversations that may otherwise go unspoken.
Hormone Therapy for Vasomotor Symptoms
Presenter: Dr. Stephanie Faubion — Mayo Clinic Slides → Meno 101 Faubion slides.pdf
What was covered Clear review of indications, contraindications, route selection, and why transdermal options may be preferred for many women.
Key takeaway The “Timing Hypothesis” is real: the benefit-risk profile of HT is most favorable when initiated closer to menopause, not decades later.
Where Amissa fits Objective vasomotor data gives providers a better understanding of whether therapy is working — or when to personalize the plan.
Management of Sexual Dysfunction at Menopause
Presenter: Dr. Sandy Falk — Dana-Farber Cancer Institute Slides → Meno 101 Falk slides.pdf
What was covered Reviewed biological, psychological, and relationship factors affecting sexual function and emphasized that clinicians should routinely screen — because most patients won’t initiate the topic.
Key takeaway Sexual health is integral health. Evidence-based solutions exist — but stigma and silence remain the primary barriers to treatment.
Where Amissa fits Patients can privately track symptoms related to sexual discomfort or interest, providing clinicians a starting point for compassionate, clinically-grounded dialogue.
Cognitive Behavioral Therapy for Menopause Symptoms
Presenter: Dr. Danette Conklin — University Hospitals Cleveland Medical Center Slides → Meno 101 Conklin slides.pdf
What was covered Evidence-based CBT protocols improve hot flashes, sleep, mood, and coping — a critical option for patients who decline or cannot take HT.
Key takeaway CBT doesn’t eliminate every flash — it reduces how much they disrupt life. That shift in perception and coping improves quality of life dramatically.
Where Amissa fits Passive physiological signals paired with self-reported “bother ratings” can identify when stress or sleep disruption drives symptoms — and prompt behavioral strategies.
Menopause 101 — Core Concepts
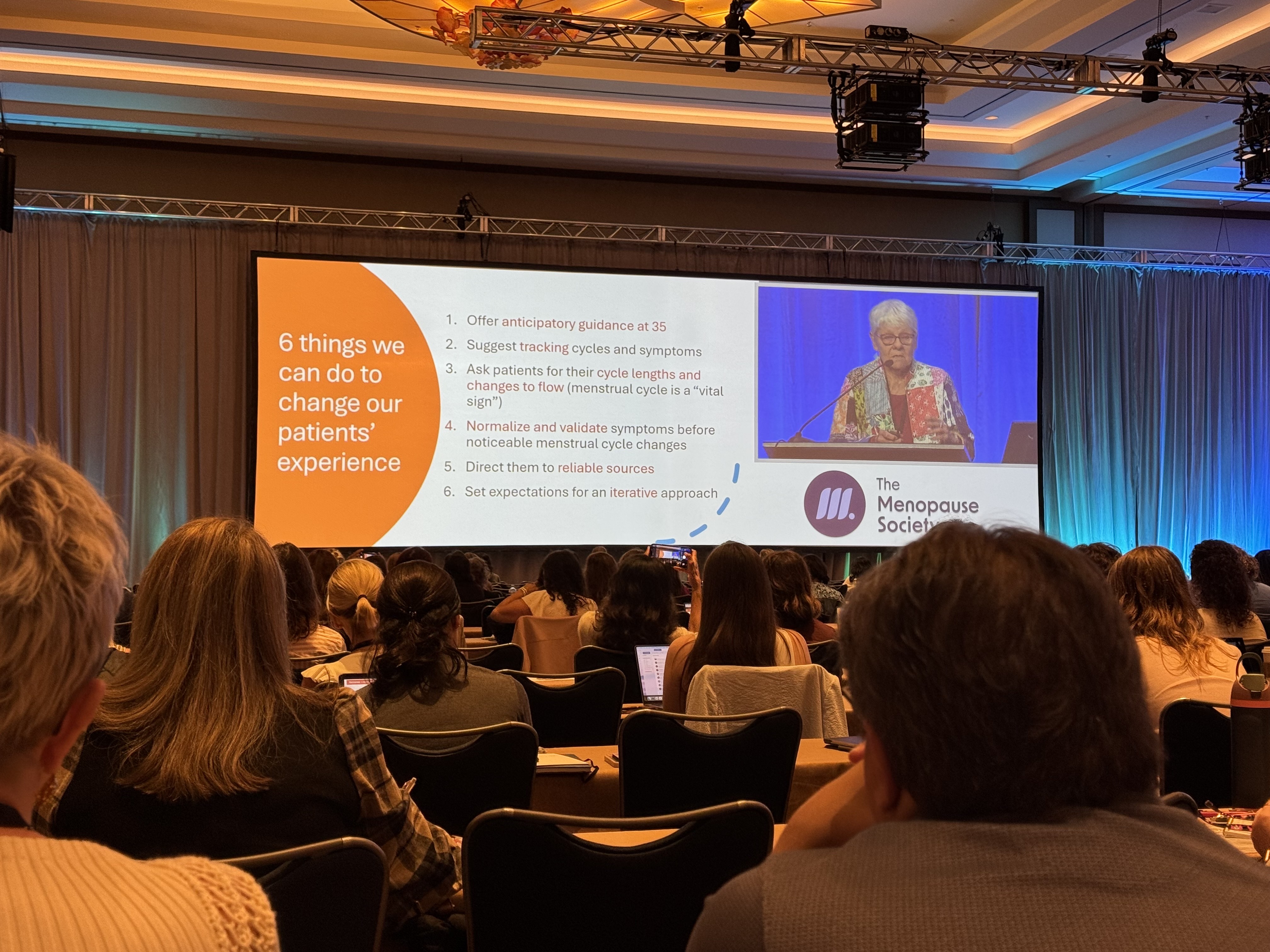
Presenter: Dr. Monica Christmas — University of Chicago Medicine Slides → Meno 101 Christmas slides (1).pdf
What was covered A foundational review: what menopause is (and isn’t), staging, terminology, and common clinical presentations — including perimenopause, where confusion and misdiagnosis often occur.
Key takeaway Perimenopause is hormonal instability — not hormonal absence — and requires nuanced evaluation to avoid unnecessary delays in symptom management.
Where Amissa fits Trend-based insights help clinicians differentiate cyclic changes from true decline in ovarian function — improving diagnosis accuracy.
Case Discussions
Facilitator: Dr. Monica Christmas Slides → Meno 101 Case Presentations Slides.pdf
What was covered Real-world scenarios covering cycle changes, mood shifts, metabolic health, and treatment sequencing over time.
Key takeaway Management is not one moment — it is a longitudinal journey. Continual monitoring ensures therapy evolves alongside the patient.
Where Amissa fits Long-term engagement supports continuity of care, especially in multi-provider environments or evolving life circumstances.
Non-Hormone Treatment Options for VMS
Presenter: Dr. Janet Carpenter — Indiana University Slides → Meno 101 Carpenter slides.pdf
What was covered Reviewed the highest-quality evidence behind non-hormonal therapies — including neurokinin B antagonists, SSRIs/SNRIs, gabapentin, oxybutynin, CBT, and more.
Key takeaway Women have more options than they’ve ever been told. Treatment should be tailored based on symptoms, risks, preferences, and response.
Where Amissa fits Monitoring wearable signals, paired with patient-reported outcomes, helps clinicians see what is truly moving the needle — across meds, behavior, and lifestyle.
Final Thoughts
From POI to sexual health to behavioral therapies and new pharmacologic advances — menopause care is expanding faster than most clinicians can keep up.
That’s why Amissa exists.
We take complex symptom patterns and physiologic data and transform them into clear, clinically-relevant insights — helping providers deliver more confident, evidence-aligned care.
If you’d like to bring these capabilities to your practice — or want a deeper dive into any of these topics — we’re here to support you.
Want support through the transition?
Sign up for early access to Amissa and stay informed as we grow.
