Only one-third of people above the age of 70 have healthy bones , and women face a significantly higher risk of bone loss and fragility than men .
The menopause transition is a critical period in which bone strength changes begin, and this can set the stage for developing osteoporosis later in life .
The good news? There are ways to reduce your risk of osteoporosis, and treatment options can help if it occurs . Understanding what happens to your body and bones during menopause and as you age is essential for long-term well-being.
Osteoporosis and menopause
Osteoporosis is a disease that weakens bones, making them more likely to fracture . Nearly one in three women will experience an osteoporotic fracture in their lifetime , and many never regain full independence afterwards .
Often called a ‘silent disease’, osteoporosis is severely underdiagnosed because it typically has no symptoms until you’re suffering from a fracture or broken bone .
What happens to bone health during the menopause transition?
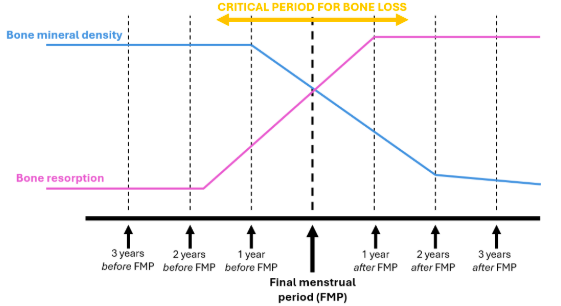
Menopause and bone density loss are linked. If untreated, bone health deteriorates quickly during the menopause transition . The key changes are a loss of bone mineral density (BMD) and bone strength. During perimenopause, bone density decreases by 10% on average .
The most critical period for bone loss is the three years surrounding the final menstrual period (FMP). Bone density loss peaks about a year and a half after your FMP .
However, you won’t know you’ve had your final period until a year after. If your goal is to prevent osteoporosis later in life, it’s never too early to take action!
What if you’ve already had your last period? Postmenopausal women continue to lose bone density gradually in the years after the FMP, so there’s still time to make changes to reduce the rate of loss.
Adapted from ; not to scale
Why does menopause cause osteoporosis?
Hormonal changes are closely associated with a decrease in bone density. A decrease in estrogen levels and an increase in follicle-stimulating hormone (FSH) during the menopause transition disrupt the balance of bone breakdown vs bone formation. As estrogen declines, bone resorption (breakdown) outpaces formation.
Risk factors for osteoporosis include:
Getting older: osteoporosis becomes a concern for most people over the age of 75, but those with ovaries face a unique increased risk after the menopause transition
Smoking cigarettes
Drinking too much alcohol: specifically, more than one standard drink per day
Diabetes (in certain bones, such as the upper femur, or thigh bone)
Race and ethnicity : for example, hip fractures are more common in white women than in Black, Hispanic, or Asian women in the United States
Severe vasomotor symptoms such as hot flashes
A family history of osteoporosis
Other life circumstances, even those that might not seem obviously connected to bone health, can also impact bone density and fracture risk. For example, non-White women with lower education levels often have a higher risk of fractures related to low bone mineral density .
This may be related to social disadvantages that make it difficult for these women to achieve an ideal peak bone mass in their late teens and early twenties: basically, their bone strength started off behind and couldn’t catch up .
More than just broken bones: How does osteoporosis impact everyday life?
Osteoporosis can have a profound impact on your daily life. Osteoporosis increases the risk of fractures from even minor falls . These injuries often lead to pain, disability, hospitalization, and reduced mobility .
After a hip fracture, many women never regain independence, and their risk of death within a year doubles .
While osteoporotic fractures, especially of the hip and the vertebrae, can be debilitating, many people still heal well from them with time and rehab . Some rehab exercises also help with future fracture prevention, since people with prior fractures are at higher risk of future fractures .
So what can you do to prevent fractures? Let’s find out.
Preventing osteoporosis: what can you do to prevent bone loss and fractures?
Bones are living tissues. They are incredibly dynamic , adapting to the stresses you put on them, and they’re quite good at healing themselves. There are many tools you can use throughout your life to promote and improve your bone strength, even if you’ve already experienced fractures.
Research studies highlight several strategies to maintain bone health during and after the menopause transition. Here are some to consider.
Maintain a healthy diet
Getting enough vitamin D and enough calcium is crucial to maintaining bone health . A well-rounded, healthy diet is an excellent starting point, as many foods contain these nutrients naturally. For example:
Dark green leafy vegetables are a good source of calcium and vitamin K, another vitamin that helps your body build and maintain bone . Certain forms of vitamin K may help improve bone density in women with osteoporosis, but we need more studies to be sure .
Fatty fish such as salmon are rich in vitamin D .
Isoflavones, compounds often found in soy products, may also support bone strength, though we need more research in this area .
Some people will benefit from additional supplements. However, you should always talk with your doctor before beginning a new supplement. This can help ensure you avoid excessive amounts of certain vitamins, including calcium and vitamin D, which can actually be harmful .
Focus on health-promoting lifestyle changes
Avoid smoking and limit alcohol consumption to fewer than two standard drinks per day . Smoking cigarettes and excessive drinking both negatively impact bone health.
Stick with regular exercise
At the right dosage and frequency, physical activity strengthens bones and decreases the risk of falls and bone fractures .
Weight-bearing exercise—think walking, dancing, weight training, etc.—promotes bone formation . Combining aerobic exercise with resistance training and balance exercises is a great way to check all your boxes !
Talk with your provider about menopause hormone therapy (MHT)
MHT, formerly known as hormone replacement therapy or HRT, is effective in maintaining bone mineral density (BMD) and preventing osteoporotic fractures in at-risk women . MHT works by reducing bone resorption, the body’s natural process of breaking down bone .
Women who discontinued MHT after the Women’s Health Initiative study (WHI) had reduced BMD, despite maintaining usual physical activity . You should discuss the individual risks and benefits of MHT with your healthcare provider.
Consider non-hormonal medication options if needed
For cases in which diet, exercise, and MHT aren’t sufficient, there are several osteoporosis medications on the market. These medications work by rebalancing bone remodeling (bone resorption vs. bone rebuilding).
However, they also have limitations and can have adverse side effects : talk to your healthcare provider to understand their risks and benefits for you.
What can you track to maintain your bone health and why?
A healthy lifestyle is key to maintaining bone health. Logging workouts with your smartwatch can help ensure you are getting a good balance of resistance and aerobic training in your schedule. Tracking your food intake can help you maintain a healthy weight and ensure you’re getting enough vitamin D and calcium in your diet .
Tracking bone health helps identify bone loss at an early stage before fractures occur. The Fracture Risk Assessment Tool (FRAX) and dual-energy x-ray absorptiometry (DXA) scan can both help predict bone mineral density .
Questions to bring to your healthcare provider
The menopause transition marks a pivotal time for your bone health, so it’s important to take an active role in maintaining it. Here are some key questions to get the conversation started:
Could I develop osteoporosis, and how does that affect the risk that I could break bones? Should I have a bone density test?
How can I rebuild bone strength and protect my bone tissue?
Should I be taking a vitamin D supplement or a calcium supplement?
What type and amount of exercise should I do? How key is weight-bearing exercise? Should I focus on lifting light weights or heavy ones?
By understanding your risks for decreased bone density and taking proactive steps to prevent osteoporosis, you can maintain bone strength and quality of life as you age. Amissa is here to support you every step of the way.
DISCLAIMER
This article is intended for educational purposes only, using publicly available information. It is not medical advice, and it should not be used for the diagnosis, treatment, or prevention of disease. Please consult your licensed medical provider regarding health questions or concerns.
Want support through the transition?
Sign up for early access to Amissa and stay informed as we grow.
