Bladder problems are quite common among most women of all ages, including those who are not yet peri- or postmenopausal. Over half of women will experience bladder symptoms at some point in their lives .
Despite how common they are, bladder issues are still an overlooked aspect of the menopause transition. Perimenopausal symptoms are more than hot flashes and changes to the menstrual cycle; many women also experience frequent urination, urgency, and other urinary symptoms.
Perimenopausal and postmenopausal women often experience worse bladder health and function compared to premenopausal women . People with bladder symptoms experience reduced quality of life and use more healthcare than peers without these issues .
Menopause symptoms are many and varied. If you’ve been asking yourself, ‘Is frequent urination a sign of menopause?’, read on.
Let’s talk about pee, baby: perimenopause and bladder issues
The Menopause Society introduced the term genitourinary syndrome of menopause (GSM) in 2014 . GSM refers to a range of urinary and vaginal symptoms caused by declining androgen and estrogen production during the menopausal transition .
GSM is quite common, affecting between 27% and 84% of postmenopausal women . Common symptoms include vaginal dryness, irritation, and urinary issues, such as bladder leaks and sudden urgency to pee.
Although urinary symptoms are core to GSM, they still don’t get as much recognition as vaginal and sexual symptoms. Urinary symptoms due to GSM may also overlap with those caused by other urologic conditions, making diagnosis and management more challenging .
Overactive bladder and menopause are also closely linked. Overactive bladder, abbreviated OAB, is the name for a group of bladder syndromes . Overactive bladder symptoms include urgency to pee, frequent urination (especially frequent nighttime urination), and incontinence.
You may experience some of these common urinary and bladder problems during menopause:
Urinary urgency: A strong, sudden urge to urinate
More frequent urination: Needing to urinate more often than usual
Nocturia: Waking during the night to urinate
Dysuria: Painful, burning, or stinging sensations when you pass urine
Recurrent urinary tract infections (UTIs): Defined as 2+ UTIs in 6 months or 3+ in a year
Urinary incontinence: Involuntary leakage of urine
Urinary incontinence comes in many forms. Three types that are common during and after the menopause transition include :
Stress incontinence: leaking urine with coughing, sneezing, or exercise–all of which can place extra pressure on the bladder
Urge incontinence: leaking urine after a sudden, intense urge to urinate, often part of overactive bladder
Mixed incontinence: when you experience both stress incontinence and urge incontinence
Does menopause cause frequent urination and other bladder problems?
It is difficult to fully separate the effects of aging from hormonal changes on the bladder. There is a clear association between the number of years since menopause and increased rates of urinary incontinence (UI) .
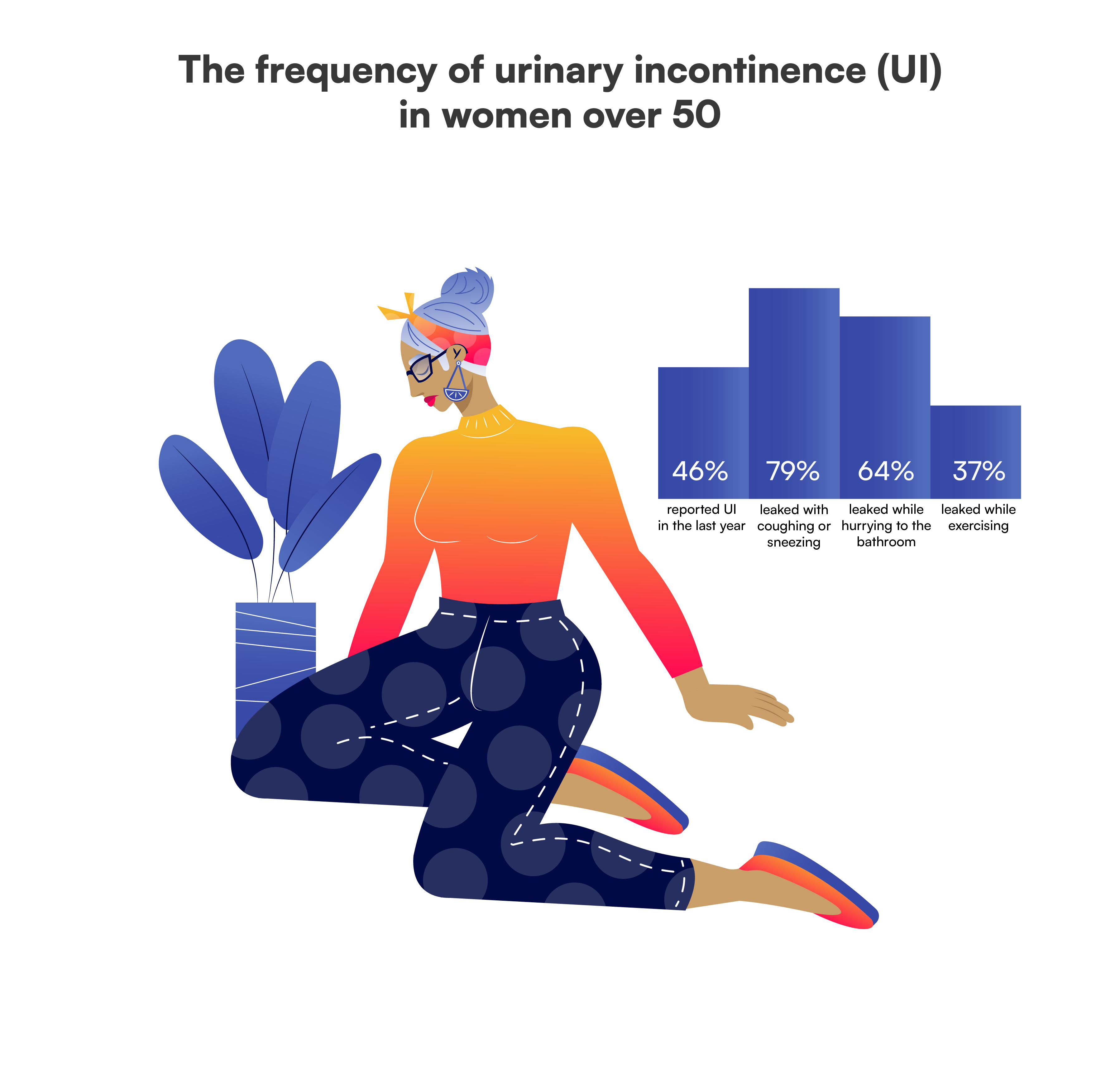
More than 50% of postmenopausal people are affected by UI . But does this association signify causation?
Estrogen plays a critical role in maintaining the health and function of the genitals and urinary tract. During menopause, the drop in estrogen levels leads to anatomical changes to the genitourinary tract .
Several genitourinary tissues change during menopause:
The pelvic floor muscles, which support the bladder and urethra, weaken. This decreases their ability to effectively control the flow of urine. This contributes to urinary retention (difficulty emptying the bladder) and urinary incontinence (involuntary leakage of urine) .
As part of the process of urogenital atrophy, the lining of the urethra thins, making it easier for urine to leak during a cough, sneeze, or when exercising .
The bladder muscles become less elastic and responsive . The vagina becomes drier and its pH decreases, which results in changes to the normal, healthy bacteria that protect the vagina. This can increase your risk of recurrent UTIs .
In addition to hormonal effects, the aging process can cause changes to your bladder health. As the bladder ages, its muscular wall weakens and tires more easily. The nerves that control it also become less responsive .
Additional risk factors for urinary incontinence include :
Obesity
Giving birth to more children, particularly through vaginal childbirth
Oral hormonal medications
Breaking the seal on bladder talk: How may this impact your day-to-day?
Bladder symptoms can significantly affect your daily life and social life :
Disrupted sleep due to nighttime pee breaks (aka nocturia)
Embarrassment or anxiety about leakage
Avoidance of social, work, or physical activities
Increased healthcare visits and costs
These issues may also impact sexual health. Women dealing with incontinence and pelvic pain often experience sexual dysfunction . GSM is usually accompanied by decreased sex hormone levels and sometimes painful intercourse, further contributing to these challenges .
This can all feel like a lot of bad news…but before you throw up your hands in defeat, consider this: there’s a long-standing myth in society that leaking urine is “just a part of getting older” or “the price you pay for having babies”.
While rates of UI are typically higher in older individuals and those who’ve completed menopause, this does not mean you have to “just live with it”. There are a lot of treatment options that can help you address and overcome bladder symptoms, no matter your age!
When you gotta go….what can you do to help?
GSM is a chronic, progressive condition, and many symptoms can worsen after menopause . Fortunately, a range of safe and effective treatment options is available. Early diagnosis and care can prevent complications and improve your physical and emotional well-being .
Traditional GSM therapies include vaginal estrogen, vaginal moisturizers, and lubricants . Some things to know about hormonal therapies for bladder symptoms:
Vaginal estrogen (local, low-dose) is highly effective at reducing urinary urgency, frequency, incontinence, and recurrent UTIs . It may also be safe for women with a history of breast cancer, but this is person-dependent: talk with your provider to understand the potential risks and benefits for your unique case.
Systemic hormone therapy (HT), however, is generally ineffective for urinary symptoms and may even worsen them . Up to 25% of systemic HT users also require vaginal estrogen to manage urogenital issues .
HT may help with nocturia, mostly by improving sleep quality .
Complementary therapies exist for those who wish to avoid hormonal treatments, including: herbal supplements, mind-body practices, educational interventions, and pelvic floor physical therapy . Always consult with your healthcare provider before starting any new supplements, because some are ineffective and may even be harmful.
In summary: For many, local vaginal estrogen is the most effective medical treatment for urinary symptoms related to GSM, especially for those who have an overactive bladder or recurrent UTIs .
Additional strategies you can use to help control urination and address bladder symptoms include:
Pelvic floor strength and coordination exercises: Improve the function of the pelvic muscles that support the bladder
Lifestyle changes: Maintain a healthy weight, and avoid bladder irritants such as caffeine and spicy foods
Bladder training: Urinate at set intervals, such as every 1-2 hours, then gradually increase the interval length
Double voiding: Urinating, waiting a few minutes, and then attempting to urinate again (without pushing or straining!)
Conscious hydration: Avoid drinking fluids within a couple of hours of bedtime
Nerve stimulation: A non-surgical option that can help control the urinary urgency and frequency
Surgery: May be an option for very severe cases
Urine for a surprise: Should you track when you go to the toilet and why?
Tracking your symptoms related to increased urgency, as well as other symptoms, is an important tool for management. It can help you:
Recognize patterns and symptom triggers (e.g., certain foods, activities, or times of day).
Measure how well treatments are working.
Give your healthcare provider valuable insights to help with diagnosis and care planning.
Although tracking might not help you track exactly when menopause occurs, it’ll help you maintain awareness and learn more about managing urinary symptoms
Don’t just hold it in: Questions to bring to your healthcare provider
Only one-third of women with incontinence seek treatment , even though it’s more common than diabetes, hypertension, or depression. Many don’t view it as a serious problem or realize help is available ...but now you know better!
Don’t hesitate to ask for help if you are struggling with bladder symptoms: clinicians hear about and help with these issues all the time!
Here are some questions you may want to ask your healthcare provider:
If I experience frequent urination or bladder leaks, is this related to menopause or another condition?
When should I be concerned about recurrent UTIs?
Should I consider local estrogen therapy for these symptoms? What are the risks and benefits?
Are there medical treatments I can use for my bladder symptoms? What lifestyle changes or exercises would be most effective to help me manage my bladder symptoms?
Bladder health is an overlooked aspect of women’s health! Understanding the causes and available treatments—and tracking your symptoms—can help you feel more in control and improve your quality of life. Amissa is here to help.
DISCLAIMER
This article is intended for educational purposes only, using publicly available information. It is not medical advice, and it should not be used for the diagnosis, treatment, or prevention of disease. Please consult your licensed medical provider regarding health questions or concerns.
Want support through the transition?
Sign up for early access to Amissa and stay informed as we grow.
